My life is a biological laboratory and I am constantly running experiments, some of them “work” but most of them fail. However, almost every experiment teaches me something, such as the experiment done over the last two weeks.
For years, I kept my insulin sensitivity very high. For example, when I eat a candy bar my blood glucose is back to baseline, and often even below baseline, after already 30 minutes. I attribute this to my low levels of body fat, strategic exercise, and metabolic hacks, including GLP-1 and leptin manipulation.
However, a consequence of high insulin sensitivity is low basal levels of insulin. Because little insulin is required to maintain blood sugar at a healthy level, little is secreted by the pancreas.
Despite of what all the “influencers” in the sphere are preaching, insulin is not exclusively bad. Sure, it drives the mTOR pathway (and therefore aging) and hyperinsulinemia is associated with all kinds of chronic diseases, such as cancer, dementia, and atherosclerosis.
But as so often, the dose makes the poison. Insulin is similar to insulin-like-growth factor 1 (IGF-1). Both of these are anabolic hormones, perhaps the most anabolic hormones known to mankind.
Insulin is also responsible for driving glucose and amino acid into cells, inducing them to be active. Furthermore, as a medium-term satiety peptides, it gives a “go-ahead” signal to the hypothalamus that the organism has plenty of resources to use for activities besides acquiring food.
When “the hormone of abundance” is very low, such as in type I diabetes, individuals basically “wither away”, both mentally and physically – in part because their cells stop metabolizing nutrients and enter a kind of “conserve resources mode”.
A normal physiological production of insulin is about 60 IU per day, 30 IU as a basal insulin (constantly trickled into the blood stream) and roughly 30 IU in response to eating food (prandial production of insulin).
So, what would happen if I, say, add 5 IU of a long-acting insulin to my physiology? Presumably not much because that would only slightly elevate my total insulin. Wrong.
Even such a low amount of insulin significantly increased my energy levels and mood – particularly on day 1 and day 2. And the change in how I felt was quite striking. Furthermore, my heart rate variability (as measured by my Oura ring) decreased by about 10 points and my resting heart rate at night increased by 5 points (from about 45bpm to about 50bpm).
All of these changes are indicators that my sympathetic nervous system activity increased. After 10 days, I then stopped the insulin injections and on that day I felt tired, “weak” and moving around was particularly onerous. The changes in resting heart rate and HRV reversed – indicating that my sympathetic nervous system output had dropped again.
I also got lightheaded multiple times, presumably because my CNS had partially adapted to the higher SNS-activity, analogous to how people feel tired and weak after having taken simulants for a couple of days and then suddenly stopping.
I then reintroduced 5 IU of insulin degludec and lo and behold, my SNS activity rose again.
Lessons
My basal insulin levels are very low – perhaps too low.
While having very low levels of insulin may be good for longevity, it may not be optimal for vitality. As so often, vitality and longevity are at odds.
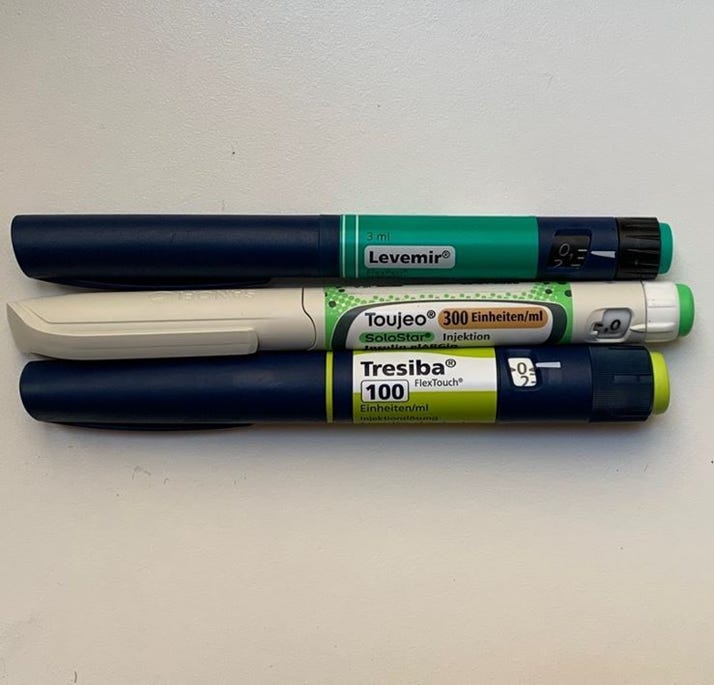
Insulin degludec had more pronounced effects that insulin glargine or insulin detemir – 3 different forms of long-acting insulins that differ in their half-lives and presumably also in their ability to cross the blood brain barrier.
The upsides and downsides of insulin
In biology, things are rarely “bad” or “good”. Insulin is no exception. I personally do not want to be “low insulin all of the time” but rather “low insulin resistance all of the time”. But before we get to that, I will briefly discuss the positive and negative aspects of insulin.
Insulin is the most anabolic hormone in the human body (hence its abuse in bodybuilding) and turns on a variety of growth pathways. While this is good for a developing organism, these growth-promoting effects also accelerate the aging process, which may be partly considered a continuation of the pre-adulthood growth program.
Chronic hyperinsulinemia, as it happens in states of insulin resistance, will cause growth pathways to be always “on”, which promotes a host of age-associated diseases such as cancer, cardiovascular disease, and neurodegeneration.
Furthermore, hyperinsulinemia inhibits lipolysis (the breakdown of triglycerides in fat tissue) and beta-oxidation (the breakdown of fatty acids for energy) while stimulating lipogenesis (the synthesis of fatty acids) and adipogenesis (the storage of fat in adipocytes), thereby promoting fat gain, which wreaks havoc on metabolic health through a variety of interdependent mechanisms. As one researcher put it: “Obese people are essentially starving in an encasement of blubber.”
Unfortunately, insulin is extensively used in the treatment of early-stage type II diabetics to keep plasma levels of glucose within a healthy range. Adding insulin to an early-stage type II diabetic patient may help with micro-vascular disease (which impairs kidney function, eye health, and brain health) but at the expense of accelerating macrovascular disease (atherosclerosis).
Unfortunately, few physicians realize that controlling blood glucose levels is only half of the job, and the other half is keeping area-under-curve insulin levels low, and injecting loads of insulin into an organism that is already teeming with insulin is probably among the worst current practices in medicine.
Despite its bad reputation, insulin serves many vital roles, and most tissues require some of it for proper function. If insulin levels are kept at very low levels for extended periods of time, many detrimental changes occur, including plummeting energy levels, organ shrinkage, and immunosuppression.
Adequate insulin levels are also necessary for vitality. Insulin stimulates energy levels from within multiple points in the central nervous system. It also stimulates cellular energy metabolism (especially glycolysis), increases hepatic and renal conversion of T4 to T3, induces hepatic IGF-1 synthesis, and it stimulates leptin secretion. Moreover, it promotes hormone bioavailability by regulating levels of hormone-binding proteins (e.g., SHBG, CBG, TBG, IGFBP-3).
With very low levels of insulin, all of these processes are impaired, and vitality often takes a hit. I discuss this in more detail in my article on ketogenic diets.
Many tissues highly depend on stimulation by insulin (e.g., kidneys, liver, endocrine organs, etc.), and if insulin levels are kept at near zero for too long and too often, many detrimental changes occur because said tissues are never adequately stimulated to grow and maintain.
Insulin’s effect on energy levels can be readily seen when patients with Type I diabetes are treated with insulin. Within the span of just a few days, their energy levels often increase dramatically.
Of note, people who are overweight in childhood will have a greater beta-cell mass and thus a greater insulin production for life. All else being equal (e.g., regardless of energy expenditure centers in the brain “getting used to” a higher weight/appetite setpoint), if someone is overweight early, they will gain fat more easily forever.